Orthopedic surgery has made big strides when it comes to managing bone defects and saving limbs that might otherwise need amputation. One standout innovation is the transverse bone transfer bracket. This device really boosts results for patients needing bone transport or distraction osteogenesis, especially in complicated situations where traditional methods fall short. Surgeons find themselves turning to this tool more often these days. It works well across different scenarios too—from helping people recover from serious trauma injuries to fixing bones that haven't healed properly after fractures. Even in cases involving birth-related deformities, the bracket helps create better long term stability while promoting natural healing processes within the body.
This article explores the clinical applications, procedural advantages, and patient outcomes associated with the transverse bone transfer bracket in orthopedic practice.
Understanding the Role of Bone Transport Techniques
What Is Distraction Osteogenesis?
Distraction osteogenesis works by creating space between bone segments so new bone can grow in the gap as they're slowly pulled apart over time. The technique was first pioneered by Dr. Gavriil Ilizarov back in the Soviet Union, and since then it's become pretty common for fixing problems like missing bone sections, legs of different lengths, or bones that just won't heal properly. Patients typically wear some kind of external frame attached to their bones, which applies gentle pulling force day after day. This mechanical stress actually tricks the body into forming new bone tissue right where we need it most after making a carefully planned cut in the bone.
Where Does the Transverse Bone Transfer Bracket Fit In?
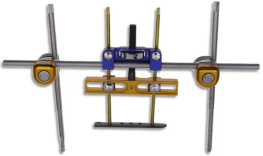
A transverse bone transfer bracket serves as a helpful tool during these procedures, allowing bones to move sideways when straight line movement just doesn't work because of how the defect is shaped or positioned. When dealing with complex fractures or unusual bone damage patterns, this device helps guide bone pieces across at right angles relative to the main length of the limb. This approach creates better bridges over gaps in the bone structure and supports proper regrowth, especially when facing those tricky situations that don't fit standard treatment models.
Key Clinical Applications in Orthopedics
Treatment of Segmental Bone Defects
When bones lose segments because of accidents, cancer removals, or infections, doctors face what many call a real puzzle. The old approaches like bone grafts or cutting off parts of the limb just don't cut it for everyone. Take bone grafting for instance, sometimes there simply isn't enough donor material available. That's where this thing called a transverse bone transfer bracket comes in handy. Surgeons can actually shift healthy bone pieces into damaged areas bit by bit while keeping everything stable during the process. This method helps maintain the original length of the limb and keeps most functions intact too, which makes all the difference for patients trying to get back to normal life after surgery.
The bracket offers an adaptable mechanical structure that ensures directional control and stability during transport. It is especially valuable when the defect lies along an oblique or non-standard axis that typical linear frames cannot adequately address.
Managing Infected Nonunions
Dealing with chronic osteomyelitis cases and those tricky infected nonunion situations usually means going through several stages of treatment first. Once doctors get rid of all the infected tissue and bring the infection under control, getting that bone back into place becomes really important. There's this thing called the transverse bone transfer bracket that helps move those broken bone pieces around exactly where they need to go, while still keeping blood flow intact and making sure everything stays fixed properly. What makes this device stand out is how it handles sideways forces on the bone, which leads to much better positioning overall and actually promotes stronger callus development even when there are big gaps between bone segments that need healing.
This device has demonstrated success in reducing healing times and improving union rates in patients with persistent infections and compromised soft tissue envelopes.
Surgical Technique and Procedural Considerations
Integration with External Fixation Systems
The transverse bone transfer bracket is most commonly used in conjunction with ring external fixators like the Ilizarov or Taylor Spatial Frame. The bracket attaches to the fixator and provides an additional axis of movement, allowing surgeons to manipulate bone transport directionally in a three-dimensional space.
Surgeons must ensure accurate frame construction and meticulous alignment to avoid joint contractures or malpositioning. The use of computer-assisted planning tools helps map the optimal trajectory for bone segment movement and bracket placement.
Customization for Anatomical Needs
Different cases require varied bracket configurations. For upper versus lower limbs, or for pediatric versus adult patients, the size and adjustment range of the bracket must be selected appropriately. Custom brackets can also be fabricated for patients with congenital deformities or post-tumor resection defects that require tailored solutions.
By combining adaptability with biomechanical strength, the transverse bone transfer bracket supports a broad range of orthopedic indications with high precision.

Advantages Over Traditional Bone Grafting Methods
Promoting Biological Healing
Unlike bone grafts, which depend on donor site viability and host integration, the transverse bone transfer technique utilizes the patientâs own osteogenic potential. The transported bone segment remains vascularized and undergoes continuous mechanical stimulation, promoting robust and natural bone formation.
This biological advantage reduces the risk of graft failure, infection, or donor site morbidityâchallenges commonly associated with allografts or autografts.
Minimizing Surgical Invasiveness
The bracket-based transport method can be performed percutaneously, reducing operative time, blood loss, and soft tissue disruption. It allows for gradual and controllable bone defect correction with fewer surgical interventions, making it especially suitable for high-risk or comorbid patients.
Postoperative Outcomes and Patient Recovery
Bone Union and Limb Function
Clinical studies have shown that patients treated with a transverse bone transfer bracket demonstrate high rates of bone union, functional limb recovery, and minimal recurrence of deformity. Callus formation typically begins within 4â6 weeks post-operatively, and consolidation progresses steadily with regular distraction adjustments.
Patients are encouraged to bear partial weight early to stimulate bone healing, and physical therapy protocols are tailored to maintain joint mobility and muscle strength during the treatment period.
Reducing Complication Rates
By allowing multi-directional transport and fine-tuned adjustment, the bracket helps avoid complications such as limb axis deviation, docking site misalignment, or soft tissue tension. When monitored closely, most patients recover without requiring additional corrective surgeries.
Conclusion â A Modern Tool for Complex Bone Reconstruction
Transverse bone transfer brackets have changed the game in orthopedic reconstruction, giving surgeons a reliable yet minimally invasive way to handle those tough bone defect cases that traditional methods struggle with. When combined with distraction osteogenesis techniques, these brackets offer something special: they allow for fine-tuned adjustments during treatment while still letting the body heal naturally. The result? Patients get back their mobility faster than before, which makes all the difference in their day-to-day lives. Many clinics report better outcomes since adopting this approach, especially when dealing with complex fractures or post-trauma reconstructions where precision matters most.
As surgical technology evolves, such tools highlight the importance of innovation in limb salvage and reconstruction strategies. For orthopedic surgeons facing complex nonunions, segmental losses, or anatomical anomalies, the transverse bone transfer bracket offers a practical and effective solution grounded in both engineering and biology.
FAQ
What conditions are best treated with a transverse bone transfer bracket?
It is most effective in managing segmental bone defects, infected nonunions, and limb deformities requiring transverse or angled bone movement.
How long does it take for the bone to regenerate using this method?
New bone formation typically starts within 4â6 weeks, with full consolidation varying by patient age, defect size, and overall healthâcommonly taking several months.
Is the procedure painful for patients?
While distraction osteogenesis involves some discomfort, pain is generally manageable with proper medications and physiotherapy. The procedure is well-tolerated by most patients.
Can this device be used in children?
Yes. Pediatric applications are common, especially in congenital deformity corrections, provided the bracket is appropriately sized and monitored for growth considerations.
Table of Contents
- Understanding the Role of Bone Transport Techniques
- Key Clinical Applications in Orthopedics
- Surgical Technique and Procedural Considerations
- Advantages Over Traditional Bone Grafting Methods
- Postoperative Outcomes and Patient Recovery
- Conclusion – A Modern Tool for Complex Bone Reconstruction
- FAQ