Intramedullary nail complications represent a significant concern in orthopedic surgery, affecting patient outcomes and recovery timelines. These complications can arise during insertion, throughout the healing process, or during long-term implant retention. Understanding the various types of intramedullary nail complications is essential for surgical planning, patient counseling, and developing effective prevention strategies. Modern orthopedic practices require comprehensive knowledge of potential adverse events to minimize risks and optimize patient care. The complexity of intramedullary nail complications demands careful consideration of patient factors, surgical technique, and implant selection to achieve successful outcomes.
Common Types of Intramedullary Nail Complications
Infection-Related Complications
Infection remains one of the most serious intramedullary nail complications, with rates varying depending on patient factors and surgical conditions. Deep infections can lead to osteomyelitis, requiring prolonged antibiotic therapy and potentially implant removal. Superficial wound infections may progress to deeper tissues if not promptly addressed. Risk factors include diabetes, smoking, immunocompromised states, and open fractures. Prevention strategies focus on sterile technique, prophylactic antibiotics, and careful patient selection.
Chronic infections represent particularly challenging intramedullary nail complications, often requiring staged procedures for resolution. Biofilm formation on implant surfaces makes eradication difficult with antibiotics alone. Surgical debridement and implant exchange may become necessary in persistent cases. Early recognition of infection signs, including elevated inflammatory markers and clinical symptoms, enables prompt intervention and better outcomes.
Mechanical Failure Events
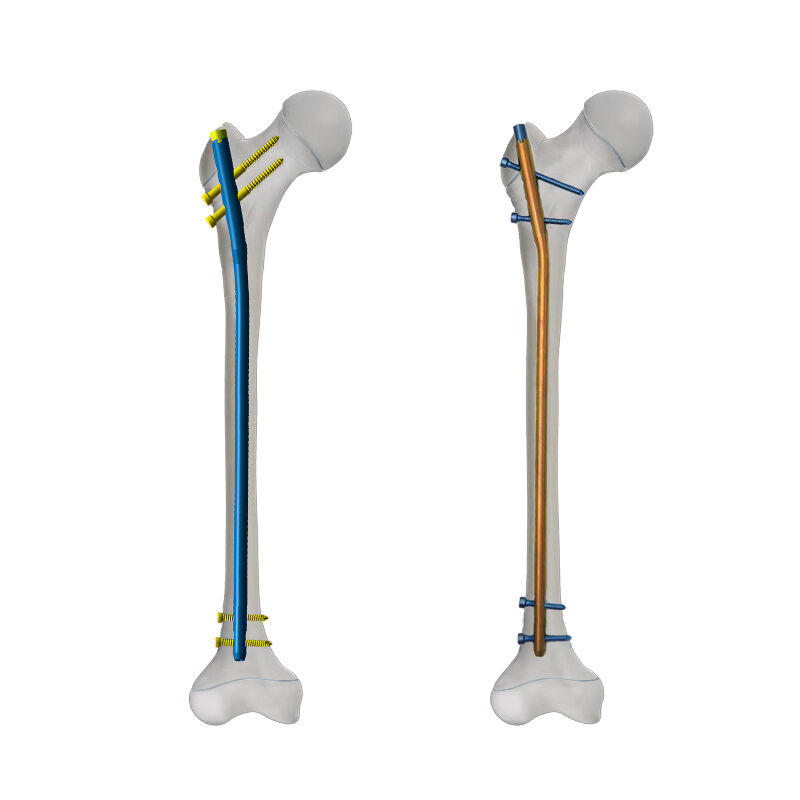
Mechanical intramedullary nail complications encompass various failure modes that compromise implant integrity and function. Nail breakage typically occurs at stress concentration points, particularly in cases of delayed union or nonunion. Screw breakage represents another common mechanical failure, especially with weight-bearing before adequate healing. These complications often require revision surgery and implant exchange for successful treatment.
Nail migration and backing out constitute additional mechanical intramedullary nail complications that affect stability and function. Inadequate initial fixation or progressive bone loss can contribute to these issues. Dynamic loading and repetitive stress cycles may gradually loosen the implant-bone interface. Prevention involves proper sizing, adequate proximal and distal fixation, and appropriate patient weight-bearing restrictions during healing phases.

Surgical Technique Impact on Complications
Entry Point Considerations
Improper entry point selection significantly influences the development of intramedullary nail complications during and after surgery. Eccentric entry points can lead to fracture propagation, cortical perforation, and suboptimal nail positioning. Anatomical variations require careful preoperative planning and intraoperative fluoroscopic guidance to ensure accurate entry point selection. Deviation from optimal entry trajectories increases the risk of secondary fractures and implant malposition.
Soft tissue damage during entry point preparation contributes to several intramedullary nail complications, including heterotopic ossification and joint stiffness. Excessive force during reaming or nail insertion can cause thermal necrosis and delayed healing. Careful technique with sharp instruments and controlled force application helps minimize these complications. Protection of surrounding structures during surgical approach reduces the risk of iatrogenic injury and associated complications.
Reaming and Nail Insertion Factors
Inappropriate reaming diameter selection creates conditions for various intramedullary nail complications related to fit and stability. Over-reaming weakens the bone and reduces cortical contact, potentially leading to instability and delayed union. Under-reaming can cause cortical fractures during nail insertion and inadequate implant seating. Optimal reaming technique balances adequate canal preparation with preservation of bone stock and endosteal blood supply.
Nail insertion force and technique directly influence the occurrence of intramedullary nail complications during the procedure. Excessive force can cause comminution at fracture sites or create new fracture lines. Improper nail advancement may result in cortical penetration or inadequate seating. Sequential reaming with gradual diameter increases reduces insertion forces and minimizes traumatic complications during implantation procedures.
Patient-Specific Risk Factors
Age and Bone Quality Considerations
Advanced age correlates with increased rates of intramedullary nail complications due to compromised bone quality and healing capacity. Osteoporotic bone provides reduced purchase for locking screws, increasing the risk of cutout and failure. Age-related changes in bone metabolism affect fracture healing rates and implant integration. Careful assessment of bone quality guides implant selection and surgical planning in elderly patients.
Pediatric patients present unique challenges regarding intramedullary nail complications due to open growth plates and ongoing bone development. Growth disturbances can occur with implants crossing physes or affecting growth centers. Size limitations may require specialized pediatric implants to avoid complications. Long-term follow-up becomes essential to monitor growth and detect late complications in developing skeletal systems.
Medical Comorbidities Impact
Diabetes significantly increases the risk of intramedullary nail complications, particularly infection and delayed healing. Hyperglycemia impairs immune function and wound healing processes, creating conditions favorable for complications. Vascular compromise associated with diabetic complications affects bone healing and implant integration. Optimal glycemic control before and after surgery helps minimize these risks and improve outcomes.
Smoking represents a major modifiable risk factor for intramedullary nail complications, affecting both healing and infection rates. Nicotine impairs bone formation and delays fracture healing, increasing the risk of nonunion and implant failure. Smoking cessation programs should be implemented before elective procedures when possible. Patient counseling regarding smoking risks helps improve compliance and reduce complication rates in orthopedic procedures.
Prevention Strategies and Best Practices
Preoperative Planning Excellence
Comprehensive preoperative assessment serves as the foundation for preventing intramedullary nail complications through careful patient selection and surgical planning. Advanced imaging studies, including computed tomography when indicated, provide detailed anatomical information for optimal implant sizing and positioning. Laboratory evaluation helps identify infection risks and metabolic abnormalities that could affect healing. Patient optimization programs address modifiable risk factors before surgery.
Template planning using preoperative imaging reduces intraoperative complications by ensuring proper implant selection and positioning. Digital templating software enables precise measurement and planning for complex cases. Backup implant availability prevents delays and suboptimal choices during surgery. Surgical team briefings review planned approaches and potential complications, ensuring coordinated responses to unexpected situations during procedures.
Intraoperative Technical Excellence
Maintaining strict sterile technique throughout the procedure significantly reduces infection-related intramedullary nail complications in all patient populations. Double gloving, frequent instrument changes, and minimal traffic patterns help minimize contamination risks. Antibiotic prophylaxis protocols should follow evidence-based guidelines for timing and agent selection. Irrigation and debridement of contaminated tissues reduces bacterial load and infection risks.
Real-time fluoroscopic guidance prevents many technical intramedullary nail complications by ensuring proper positioning and alignment throughout the procedure. Multiple fluoroscopic views confirm adequate reduction and implant placement before final fixation. Careful attention to screw placement prevents cortical perforation and neurovascular injury. Quality control measures throughout surgery help identify and correct potential problems before completion.
Management of Established Complications
Early Recognition and Intervention
Prompt recognition of developing intramedullary nail complications enables early intervention and improved outcomes for affected patients. Regular clinical and radiographic follow-up protocols help detect problems before they become severe or irreversible. Warning signs including persistent pain, swelling, drainage, or radiographic changes warrant immediate evaluation and appropriate treatment measures. Early intervention strategies often prevent progression to more serious complications requiring major revision procedures.
Diagnostic imaging plays a crucial role in evaluating suspected intramedullary nail complications and guiding treatment decisions. Serial radiographs document healing progress and identify implant problems such as loosening or migration. Advanced imaging including computed tomography or magnetic resonance imaging may be necessary for complex cases. Laboratory studies help differentiate infectious from mechanical complications and guide antibiotic selection when indicated.
Revision Surgery Considerations
Revision procedures for failed intramedullary nail complications require careful planning and specialized techniques to achieve successful outcomes. Implant removal may be challenging due to bone ingrowth or mechanical factors requiring specialized instruments. Alternative fixation methods may be necessary depending on bone stock and previous hardware placement. Patient counseling regarding revision surgery risks and expected outcomes helps set appropriate expectations for recovery.
Timing of revision surgery for intramedullary nail complications depends on various factors including infection status, bone healing, and patient symptoms. Early revision may be indicated for mechanical failures or progressive complications, while delayed approaches may be appropriate for certain infection cases. Staged procedures may be necessary for complex revisions involving infection management and bone reconstruction. Multidisciplinary consultation often benefits complex revision cases requiring specialized expertise.
Long-Term Outcomes and Monitoring
Functional Recovery Patterns
Long-term functional outcomes following intramedullary nail complications vary significantly depending on the type and severity of complications encountered. Infection-related complications generally have poorer functional outcomes compared to mechanical failures due to bone and soft tissue damage. Return to activities of daily living typically occurs gradually over months, with some patients experiencing persistent limitations. Rehabilitation programs play crucial roles in optimizing functional recovery after complication management.
Quality of life measures provide important insights into patient experiences following intramedullary nail complications and their management. Pain scores, activity levels, and patient satisfaction indices help evaluate treatment success beyond radiographic healing. Psychological factors including depression and anxiety may affect recovery patterns and require appropriate intervention. Patient support groups and counseling resources can provide valuable assistance during recovery phases.
Follow-Up Protocol Development
Systematic long-term follow-up protocols help detect late intramedullary nail complications and ensure optimal patient outcomes over time. Regular clinical examinations assess functional recovery, implant integrity, and potential problems requiring intervention. Standardized imaging schedules monitor bone healing and detect implant-related changes that may indicate developing complications. Documentation systems track outcomes and complications to improve future patient care.
Patient education regarding warning signs of potential intramedullary nail complications empowers individuals to seek prompt medical attention when problems arise. Written instructions and contact information ensure patients know when and how to report concerning symptoms. Regular communication between patients and healthcare providers maintains vigilance for potential problems. Shared decision-making regarding activity restrictions and lifestyle modifications helps prevent complications while maintaining quality of life.
FAQ
What are the most common early signs of intramedullary nail complications
Early signs of intramedullary nail complications include persistent or increasing pain, swelling, warmth, and redness around the surgical site. Drainage from the incision, fever, and difficulty with weight-bearing may indicate infection or mechanical problems. Changes in range of motion or function should prompt immediate medical evaluation. Patients should contact their healthcare provider if any concerning symptoms develop, as early intervention often prevents more serious complications from occurring.
How long does recovery typically take when intramedullary nail complications occur
Recovery time following intramedullary nail complications varies significantly depending on the type and severity of the complication. Minor complications may add several weeks to the typical healing process, while major complications requiring revision surgery can extend recovery by many months. Infection-related complications generally require longer recovery periods due to the need for antibiotic treatment and potential implant removal. Most patients can expect gradual improvement over 6-12 months following successful complication management.
Can intramedullary nail complications be prevented entirely
While intramedullary nail complications cannot be prevented entirely, their risk can be significantly reduced through proper patient selection, surgical technique, and postoperative care. Careful preoperative planning, sterile technique, and appropriate implant selection help minimize complication rates. Patient factors such as smoking cessation, diabetes control, and compliance with activity restrictions also influence complication development. Even with optimal care, some complications may still occur due to unpredictable factors or patient-specific characteristics.
When should patients seek immediate medical attention for potential complications
Patients should seek immediate medical attention for severe pain, signs of infection including fever and drainage, or sudden changes in function or mobility. Any concerning changes in the appearance of the surgical site, including increased swelling, redness, or warmth, warrant prompt evaluation. Difficulty with weight-bearing or new onset of mechanical symptoms should be assessed quickly to prevent progression of potential complications. Emergency care may be necessary for signs of severe infection or implant failure requiring urgent intervention.