Revolutionary Advances in Spine Surgery Through Modern Fixation Systems
The evolution of spinal surgery has taken a significant leap forward with the introduction of advanced spinal internal fixation systems. These innovative medical devices have transformed the way surgeons approach spinal instability and deformity correction. The posterior nail rod system, in particular, represents a groundbreaking development in spine surgery, offering enhanced stability and improved patient outcomes. As medical technology continues to advance, these sophisticated fixation systems are becoming increasingly crucial in addressing complex spinal conditions.
Understanding the Mechanics of Posterior Spinal Fixation
Core Components and Design Features
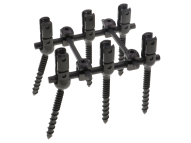
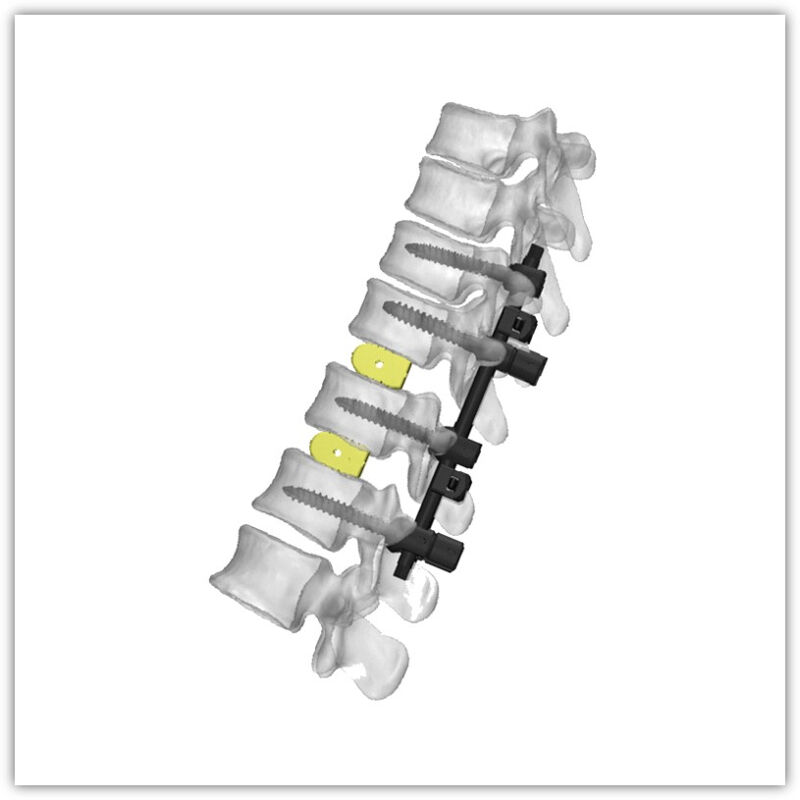
The spinal internal fixation system consists of carefully engineered components working in harmony to provide optimal spine stabilization. At its core, the posterior nail rod system utilizes specialized rods, screws, and connectors manufactured from biocompatible materials. These components are designed to withstand significant biomechanical stress while maintaining their structural integrity over time. The system's modular design allows surgeons to customize the configuration based on individual patient anatomy and specific pathological conditions.
Advanced materials science plays a crucial role in the development of these systems. Titanium alloys and other high-grade materials ensure both strength and compatibility with the human body. The surface treatment of these components promotes osseointegration, allowing for better long-term stability and reduced risk of implant failure.
Biomechanical Principles and Stability
The posterior nail rod system operates on sophisticated biomechanical principles that ensure optimal load distribution across the spine. By creating a stable construct that mimics natural spinal mechanics, the system provides immediate stability while promoting proper healing. The multi-axial capabilities of the screws allow for precise adjustment and optimal alignment, crucial for achieving desired clinical outcomes.
Engineers have incorporated cutting-edge design features that address previous limitations in spinal fixation. The system's low-profile design minimizes tissue disruption while maintaining robust mechanical properties. This advancement represents a significant improvement over traditional fixation methods, offering enhanced stability without compromising patient comfort.
Clinical Applications and Surgical Techniques
Surgical Planning and Implementation
Successful implementation of the spinal internal fixation system requires meticulous surgical planning and expertise. Surgeons utilize advanced imaging technologies and computer-assisted navigation systems to ensure precise placement of components. The posterior approach allows for optimal visualization and access to the spine, enabling surgeons to address various pathological conditions effectively.
The surgical technique involves careful consideration of patient-specific factors, including bone quality, anatomical variations, and the extent of spinal instability. Modern surgical protocols emphasize minimally invasive approaches when possible, reducing tissue trauma and accelerating recovery times.
Treatment Indications and Patient Selection
The versatility of the posterior nail rod system makes it suitable for treating various spinal conditions. Common indications include degenerative disc disease, spinal fractures, scoliosis, and other deformities requiring stabilization. Careful patient selection is crucial for optimal outcomes, considering factors such as bone quality, overall health status, and specific pathological conditions.
Surgeons must evaluate each case individually, taking into account the patient's age, activity level, and expectations. The system's adaptability allows for customized treatment approaches, ensuring the best possible outcomes for each patient's unique situation.
Advanced Features and Technological Innovations
Integration with Modern Imaging Systems
The spinal internal fixation system incorporates features that enhance its compatibility with modern imaging technologies. Radio-opaque markers and materials allow for precise intraoperative visualization and post-operative monitoring. This integration enables surgeons to achieve optimal implant positioning and verify proper alignment during the procedure.
Advanced imaging capabilities also facilitate long-term follow-up and assessment of fusion progress. The system's design allows for clear visualization on various imaging modalities, including CT and MRI, essential for monitoring patient progress and identifying potential complications early.
Smart Technology Integration
Recent developments in spinal internal fixation systems include the integration of smart technology features. Sensors embedded within the components can provide real-time data about load distribution and implant integrity. This technological advancement allows for more precise monitoring of healing progress and early detection of potential issues.
The incorporation of smart materials and surface treatments enhances the system's biological performance. These innovations promote better bone integration and reduce the risk of complications, leading to improved long-term outcomes for patients.
Clinical Outcomes and Patient Benefits
Recovery and Rehabilitation Protocols
The implementation of the spinal internal fixation system is accompanied by comprehensive rehabilitation protocols. These protocols are designed to optimize recovery while ensuring the stability of the surgical construct. Early mobilization, when appropriate, helps prevent complications and promotes faster return to normal activities.
Physical therapy plays a crucial role in the recovery process, focusing on strengthening core muscles and improving spinal mobility. The system's stability allows for more aggressive rehabilitation protocols when indicated, potentially leading to faster recovery times.
Long-term Results and Patient Satisfaction
Clinical studies have demonstrated impressive long-term outcomes with modern spinal internal fixation systems. Patients report significant improvements in pain levels, mobility, and overall quality of life. The durability of the system ensures sustained stability, while its design minimizes the risk of adjacent segment degeneration.
Follow-up studies show high patient satisfaction rates, with many individuals returning to normal activities within expected timeframes. The system's reliability and effectiveness have made it a preferred choice for both surgeons and patients seeking long-term solutions for spinal stability.
Frequently Asked Questions
What makes the posterior nail rod system different from traditional spinal fixation methods?
The posterior nail rod system offers several advantages over traditional methods, including enhanced stability, lower profile design, and improved biomechanical properties. Its modular nature allows for more precise customization to patient anatomy, while advanced materials and surface treatments promote better integration with surrounding tissues.
How long is the typical recovery period after spinal internal fixation surgery?
Recovery time varies depending on individual factors such as the extent of surgery, overall health, and compliance with rehabilitation protocols. Most patients can expect initial recovery within 4-6 weeks, with full recovery and return to normal activities typically occurring within 3-6 months post-surgery.
What is the expected lifespan of a spinal internal fixation system?
Modern spinal internal fixation systems are designed for long-term durability, with many lasting the patient's lifetime. The use of advanced materials and precise engineering ensures the system maintains its structural integrity while promoting proper spinal fusion and stability over time.