Children's bones present unique challenges that require specialized approaches in orthopedic surgery. Unlike adult skeletal structures, pediatric bones are constantly growing, adapting, and remodeling throughout development. When fractures or deformities occur in young patients, traditional adult fixation methods often prove inadequate or potentially harmful to future growth. This fundamental difference has led to the development of sophisticated pediatric internal fixation systems that address the specific biomechanical and physiological needs of growing bones. Understanding these specialized requirements is crucial for orthopedic surgeons, medical device engineers, and healthcare professionals working with pediatric populations.
Anatomical Differences Between Pediatric and Adult Bones
Growth Plate Considerations
The presence of growth plates, or physes, represents the most significant anatomical difference between pediatric and adult skeletal systems. These cartilaginous regions are responsible for longitudinal bone growth and remain active until skeletal maturity is reached, typically between ages 14-18 depending on the specific bone and individual development patterns. Growth plates are particularly vulnerable to trauma and surgical intervention, making their preservation paramount in any pediatric orthopedic procedure. When designing pediatric internal fixation systems, engineers must account for the need to avoid crossing these critical growth centers whenever possible.
The metaphyseal and epiphyseal regions adjacent to growth plates have different mechanical properties compared to the diaphyseal cortical bone found in the shaft regions. This variation in bone density and strength throughout the developing skeleton requires fixation devices that can accommodate these differences while maintaining adequate stability for healing. Modern pediatric internal fixation systems incorporate features that distribute loads appropriately across these varying bone densities, preventing stress concentration that could lead to complications or growth disturbances.
Bone Composition and Remodeling Capacity
Pediatric bones contain a higher proportion of organic matrix compared to adult bones, resulting in increased flexibility and different fracture patterns. Children's bones are more likely to bend rather than break completely, leading to unique injury types such as greenstick fractures, torus fractures, and plastic deformation injuries. This increased flexibility must be considered when selecting appropriate fixation methods, as overly rigid constructs can create stress shielding effects that interfere with normal bone development and remodeling processes.
The remarkable remodeling capacity of pediatric bones allows for correction of minor angular deformities and restoration of normal anatomy over time. However, this same remodeling potential means that inadequate fixation can result in progressive deformity if the healing environment is not properly controlled. Pediatric internal fixation systems must provide sufficient stability to maintain reduction while allowing controlled motion that promotes healthy bone formation and remodeling throughout the healing process.
Biomechanical Principles in Pediatric Fixation Design
Load Distribution and Stress Management
Effective pediatric internal fixation systems must distribute mechanical loads in ways that promote healing while protecting critical growth structures. The smaller size and different mechanical properties of pediatric bones require fixation devices with modified geometries and material properties compared to adult implants. Load distribution becomes particularly critical in metaphyseal regions where the transition from dense cortical bone to more porous cancellous bone creates potential weak points that could lead to implant failure or bone damage.
Advanced finite element analysis and biomechanical testing have revealed that traditional scaling-down of adult implant designs often results in inappropriate stress concentrations in pediatric applications. Instead, purpose-built pediatric internal fixation systems utilize optimized cross-sectional geometries, strategic placement of fixation points, and carefully engineered flexibility characteristics that match the mechanical environment of growing bones. These design modifications help prevent complications such as stress shielding, implant loosening, and growth disturbances that can occur when adult-oriented fixation principles are applied to pediatric patients.
Dynamic Stability Concepts
Unlike adult bones that primarily require static stability for healing, pediatric bones benefit from controlled dynamic loading that stimulates healthy bone formation and remodeling. This concept has led to the development of pediatric internal fixation systems that provide what is known as relative stability, allowing controlled micromotion at the fracture site while preventing gross displacement or angulation. This approach promotes callus formation and enhances the natural healing processes that are particularly robust in pediatric populations.
The implementation of dynamic stability principles requires careful consideration of implant design parameters such as working length, diameter, and material properties. Modern pediatric fixation systems often incorporate features such as optimized nail diameters that provide adequate strength while minimizing the cross-sectional area occupied within the medullary canal. This design philosophy allows for continued growth of the bone around the implant while maintaining the structural integrity necessary for successful healing outcomes.
Material Science and Biocompatibility Considerations
Titanium Alloys and Surface Treatments
Material selection for pediatric internal fixation systems requires careful consideration of biocompatibility, mechanical properties, and long-term behavior within the growing skeletal environment. Titanium and titanium alloys have emerged as preferred materials due to their excellent biocompatibility profile, corrosion resistance, and mechanical properties that more closely match those of bone compared to stainless steel alternatives. The lower elastic modulus of titanium alloys helps reduce stress shielding effects that can interfere with normal bone development and remodeling processes.
Surface treatments and coating technologies play crucial roles in optimizing the interface between pediatric implants and surrounding bone tissue. Advanced surface modifications such as plasma spray coatings, anodization treatments, and bioactive surface preparations can enhance osseointegration while maintaining the ability to remove implants when necessary. These surface technologies must be carefully balanced in pediatric applications, as permanent integration may not be desirable in cases where implant removal is planned after healing completion or when accommodating continued growth requires implant modification or replacement.
Biodegradable and Temporary Fixation Options
The development of biodegradable materials for pediatric internal fixation represents an exciting frontier that addresses many of the unique challenges associated with growing bones. Polymers such as polylactic acid, polyglycolic acid, and their copolymers offer the potential for temporary fixation that gradually dissolves as the bone heals, eliminating the need for secondary removal procedures. However, the degradation kinetics must be carefully matched to the healing timeline of pediatric bones, and the mechanical properties must be sufficient to provide adequate stability throughout the critical healing period.
Current research in biodegradable pediatric fixation focuses on optimizing material compositions and processing techniques to achieve predictable degradation profiles while maintaining adequate mechanical performance. These materials must also demonstrate excellent biocompatibility and produce non-toxic degradation products that can be safely metabolized or eliminated by the body. While biodegradable options show great promise, they currently remain limited to specific applications where the mechanical demands are relatively modest and the healing timeline is well-defined.
Clinical Applications and Surgical Techniques
Fracture Pattern-Specific Approaches
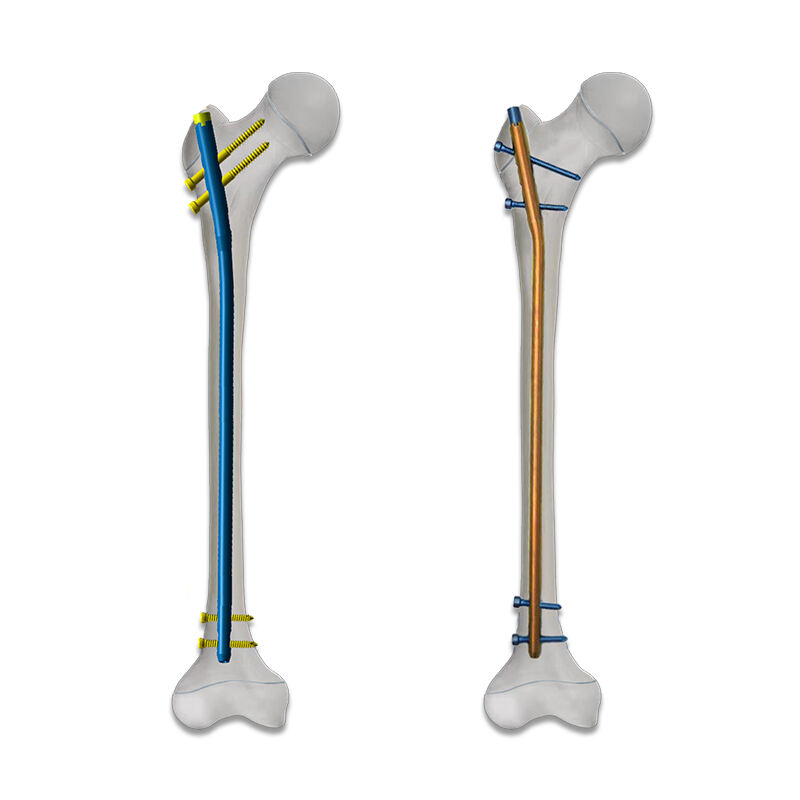
Different pediatric fracture patterns require tailored approaches using specialized internal fixation systems designed for specific anatomical regions and injury types. Femoral shaft fractures in children, for example, benefit from flexible intramedullary nailing techniques that provide stability while allowing continued growth and remodeling. These systems typically employ smaller diameter nails with optimized flexibility characteristics that can accommodate the unique mechanical environment of the pediatric femur while providing adequate fracture stabilization.
Metaphyseal fractures near growth plates present particular challenges that require fixation systems capable of providing stability without crossing or damaging the physis. Specialized implants such as metaphyseal plates with angular stability or cannulated screws placed in specific orientations allow surgeons to achieve adequate fixation while respecting the critical growth structures. The design of these specialized pediatric internal fixation systems incorporates features that facilitate precise placement and minimize the risk of growth disturbances or other complications.
Minimally Invasive Surgical Approaches
The development of minimally invasive surgical techniques for pediatric orthopedic procedures has driven innovations in internal fixation system design. Smaller incisions, reduced soft tissue trauma, and faster recovery times are particularly beneficial in pediatric populations where minimizing surgical morbidity and preserving normal development are paramount concerns. Specialized instrumentation and implant design features enable surgeons to achieve precise placement and optimal fixation through minimal access approaches.
Advanced imaging technologies and navigation systems work in conjunction with purpose-designed pediatric internal fixation systems to enable highly precise implant placement while minimizing radiation exposure to young patients. These technological advances have made it possible to achieve excellent clinical outcomes with reduced surgical trauma and improved patient experience. The integration of these technologies continues to drive further innovations in pediatric fixation system design and surgical technique development.
Growth Accommodation and Long-term Considerations
Implant Removal Strategies
Unlike many adult orthopedic implants that remain permanently in place, pediatric internal fixation systems are often designed with the expectation of eventual removal once healing is complete and growth considerations warrant implant extraction. This requirement influences design features such as material selection, surface treatments, and fixation mechanisms that must provide adequate stability during healing while facilitating safe and effective removal when indicated. The timing of implant removal must balance the benefits of maintaining fixation with the potential risks of leaving implants in place during continued skeletal growth.
Removal considerations also influence the design of specialized instrumentation and surgical techniques required for safe implant extraction. Pediatric internal fixation systems often incorporate features that facilitate removal procedures, such as optimized thread patterns on screws, standardized connection interfaces for extraction tools, and materials that resist corrosion or tissue ingrowth that could complicate removal. These design considerations ensure that when implant removal becomes necessary, it can be accomplished safely and effectively with minimal additional surgical trauma.
Monitoring Growth and Development
Long-term follow-up protocols for patients with pediatric internal fixation systems must account for the ongoing growth and development that continues after implant placement. Regular radiographic monitoring helps assess not only fracture healing but also the relationship between the implant and surrounding growth structures over time. This monitoring may reveal the need for implant modification, removal, or replacement as the child continues to grow and develop.
Advanced imaging techniques and growth prediction models help clinicians anticipate potential complications and plan appropriate interventions. The design of pediatric internal fixation systems increasingly incorporates features that facilitate this long-term monitoring, such as radiopaque markers that enable precise assessment of implant position relative to anatomical landmarks and growth centers. This ongoing surveillance ensures that any necessary interventions can be planned and executed at optimal times to minimize impact on the child's development and functional outcomes.
Future Developments and Emerging Technologies
Smart Implant Technologies
The integration of smart technologies into pediatric internal fixation systems represents an exciting frontier that could revolutionize the monitoring and management of healing in young patients. Sensor-embedded implants capable of monitoring load transmission, bone healing progress, and implant integrity in real-time could provide unprecedented insights into the healing process and enable more precise treatment adjustments. These technologies must be adapted to the unique requirements of pediatric applications, including miniaturization constraints and the need for long-term biocompatibility in the growing skeletal environment.
Wireless communication capabilities and advanced data analytics could enable continuous monitoring of healing progress without the need for frequent radiographic examinations, reducing radiation exposure while providing more detailed information about the healing process. However, the implementation of these technologies in pediatric applications requires careful consideration of power requirements, biocompatibility, and the potential effects on normal growth and development processes.
Personalized Medicine Approaches
Advances in medical imaging, 3D printing, and computational modeling are enabling increasingly personalized approaches to pediatric internal fixation. Patient-specific implants designed using advanced imaging data and biomechanical modeling can optimize fit, function, and healing outcomes for individual patients. This personalized approach is particularly valuable in pediatric applications where anatomical variations and growth patterns can significantly influence treatment outcomes.
The development of rapid prototyping and manufacturing technologies makes it increasingly feasible to produce customized pediatric internal fixation systems for complex cases or unusual anatomical configurations. These personalized solutions can address specific patient needs while maintaining the proven design principles that ensure safe and effective treatment outcomes. As these technologies continue to advance and become more accessible, they promise to further improve the precision and effectiveness of pediatric orthopedic treatments.
FAQ
What makes pediatric internal fixation systems different from adult implants?
Pediatric internal fixation systems are specifically designed to accommodate the unique characteristics of growing bones, including the presence of growth plates, different mechanical properties, and ongoing remodeling processes. These systems typically feature smaller sizes, optimized flexibility, and design elements that avoid interference with growth centers while providing adequate stability for healing.
How do surgeons determine when to remove pediatric internal fixation implants?
The timing of implant removal depends on multiple factors including fracture healing status, patient age, growth remaining, implant type, and potential complications. Generally, removal is considered once healing is complete and continued presence of the implant may interfere with normal growth or cause other problems. This decision requires careful evaluation of risks and benefits for each individual patient.
Are there any long-term risks associated with pediatric internal fixation systems?
While pediatric internal fixation systems are generally safe and effective, potential long-term risks include growth disturbances if growth plates are affected, implant-related complications such as loosening or breakage, and the need for additional surgeries for implant removal or revision. Regular follow-up monitoring helps identify and address any potential issues early in their development.
What role do biodegradable materials play in pediatric orthopedic surgery?
Biodegradable materials offer the potential advantage of providing temporary fixation that dissolves as healing progresses, eliminating the need for removal surgery. However, their use is currently limited to specific applications where mechanical demands are modest and healing timelines are predictable. Ongoing research continues to expand the potential applications of these materials in pediatric orthopedics.
Table of Contents
- Anatomical Differences Between Pediatric and Adult Bones
- Biomechanical Principles in Pediatric Fixation Design
- Material Science and Biocompatibility Considerations
- Clinical Applications and Surgical Techniques
- Growth Accommodation and Long-term Considerations
- Future Developments and Emerging Technologies
-
FAQ
- What makes pediatric internal fixation systems different from adult implants?
- How do surgeons determine when to remove pediatric internal fixation implants?
- Are there any long-term risks associated with pediatric internal fixation systems?
- What role do biodegradable materials play in pediatric orthopedic surgery?


