The Evolution of Surgical Fixation Devices in Modern Medicine
In the realm of orthopedic surgery, the advancement of medical technology has revolutionized how we approach bone fixation and reconstruction. At the forefront of these innovations are orthopedic screws, sophisticated medical devices that have become fundamental tools in surgical procedures. These precision-engineered components play a crucial role in stabilizing fractures, supporting joint replacements, and facilitating proper bone healing.
Modern orthopedic screws represent decades of medical research and technological refinement. Their development has transformed the field of orthopedic surgery, enabling procedures that were once impossible and improving patient outcomes across countless surgical applications. The strategic selection and placement of these specialized implants can mean the difference between optimal healing and potential complications.
Essential Categories of Surgical Fixation Hardware
Cortical Bone Screws
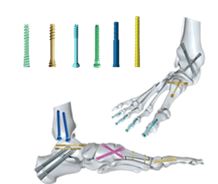
Cortical bone screws are specifically designed for use in the dense outer layer of bone tissue. These orthopedic screws feature a narrow thread pattern and sharp cutting flutes that allow for precise insertion into compact bone structure. Their design typically includes a shallow thread depth and smaller pitch, making them ideal for situations requiring maximum holding power in harder bone tissue.
The application of cortical screws requires careful consideration of factors such as bone density, required compression force, and anatomical location. Surgeons often select these screws for diaphyseal fixation, where the bone's cortical layer is thickest and strongest.
Cancellous Bone Screws
In contrast to cortical screws, cancellous orthopedic screws are engineered for use in softer, spongier bone tissue. These screws feature wider thread patterns and deeper threads that provide superior grip in less dense bone material. The design allows for greater surface area contact, distributing forces more evenly across the surrounding tissue.
Cancellous screws are particularly valuable in metaphyseal and epiphyseal regions of long bones, where the internal structure is predominantly trabecular. Their unique thread configuration helps prevent pull-out and ensures stable fixation even in compromised bone quality.
Advanced Design Features in Modern Fixation Systems
Self-Tapping Technology
Modern orthopedic screws often incorporate self-tapping features that eliminate the need for pre-threading of the bone. This innovation reduces surgical time and minimizes trauma to surrounding tissue. Self-tapping screws include specialized cutting flutes at their tips, allowing them to create their own thread pattern as they are inserted.
The efficiency of self-tapping designs has made them increasingly popular in orthopedic procedures. These screws provide surgeons with greater control during insertion while maintaining the structural integrity of the surrounding bone.
Variable-Angle Locking Mechanisms
Variable-angle locking orthopedic screws represent a significant advancement in fixation technology. These sophisticated implants allow surgeons to select the optimal angle for screw placement while maintaining the security of a locked construct. The ability to customize screw trajectory while ensuring stable fixation has expanded the possibilities for complex fracture patterns and reconstructive procedures.
The locking mechanism prevents screw toggle and maintains rigid fixation even in osteoporotic bone. This technology has proven particularly valuable in periarticular fractures and revision surgeries where conventional fixation methods may be challenging.
Material Composition and Biocompatibility
Titanium Alloy Components
Titanium alloys have become the gold standard for orthopedic screws due to their exceptional strength-to-weight ratio and biocompatibility. These materials demonstrate remarkable resistance to corrosion and fatigue, ensuring long-term stability of the fixation construct. The reduced modulus of elasticity compared to traditional stainless steel helps prevent stress shielding and promotes healthy bone remodeling.
Advanced surface treatments and coatings can further enhance the performance of titanium orthopedic screws. These modifications may improve osseointegration, reduce the risk of infection, or facilitate easier removal if required at a later date.
Bioabsorbable Options
Recent innovations have led to the development of bioabsorbable orthopedic screws that gradually dissolve as healing progresses. These implants eliminate the need for secondary removal surgery and reduce the long-term presence of foreign material in the body. The controlled degradation process is designed to match the natural healing timeline of bone tissue.
While not suitable for all applications, bioabsorbable screws have found particular utility in pediatric orthopedics and sports medicine procedures. Their use continues to expand as material science advances and long-term clinical data supports their efficacy.
Clinical Applications and Surgical Considerations
Fracture Fixation Principles
The successful use of orthopedic screws in fracture fixation requires a thorough understanding of biomechanical principles and healing biology. Proper screw selection and placement must account for fracture pattern, bone quality, and anticipated loading conditions. Surgeons must carefully balance the need for rigid fixation against the risk of compromising local blood supply and bone integrity.
Modern surgical techniques often combine different types of orthopedic screws with plates or other fixation devices to create stable constructs that promote optimal healing. The strategic use of compression and neutralization screws can help achieve both primary and secondary bone healing.
Arthroplasty and Reconstruction
In joint replacement and reconstructive procedures, orthopedic screws play a vital role in securing prosthetic components and augmenting bone stock. The selection of appropriate screws must consider factors such as bone quality, anatomical constraints, and the potential need for future revision surgery.
Advanced imaging and surgical planning tools have enhanced the precision of screw placement in complex reconstructive cases. Computer-assisted navigation and patient-specific guides help ensure optimal implant positioning and minimize the risk of complications.
Frequently Asked Questions
What determines the choice between different types of orthopedic screws?
The selection of orthopedic screws depends on multiple factors including bone quality, anatomical location, type of fracture or reconstruction needed, and anticipated mechanical loads. Surgeons consider the specific characteristics of cortical versus cancellous bone, required compression forces, and whether locking or non-locking fixation is appropriate for the clinical situation.
How long do orthopedic screws typically remain in place?
The duration orthopedic screws remain implanted varies significantly based on the specific procedure and patient factors. In many cases, screws are permanent implants designed to remain in place indefinitely. However, in certain situations, particularly with pediatric patients or temporary fixation needs, screws may be removed once healing is complete, typically after 12-18 months.
What recent innovations have improved orthopedic screw technology?
Recent advances include the development of variable-angle locking systems, enhanced surface treatments for better osseointegration, smart sensors for monitoring healing progress, and bioabsorbable materials. Additionally, improved manufacturing processes have led to stronger, more precise implants with better handling characteristics for surgeons.

