The Role of Intramedullary Nails in Modern Orthopedic Surgery
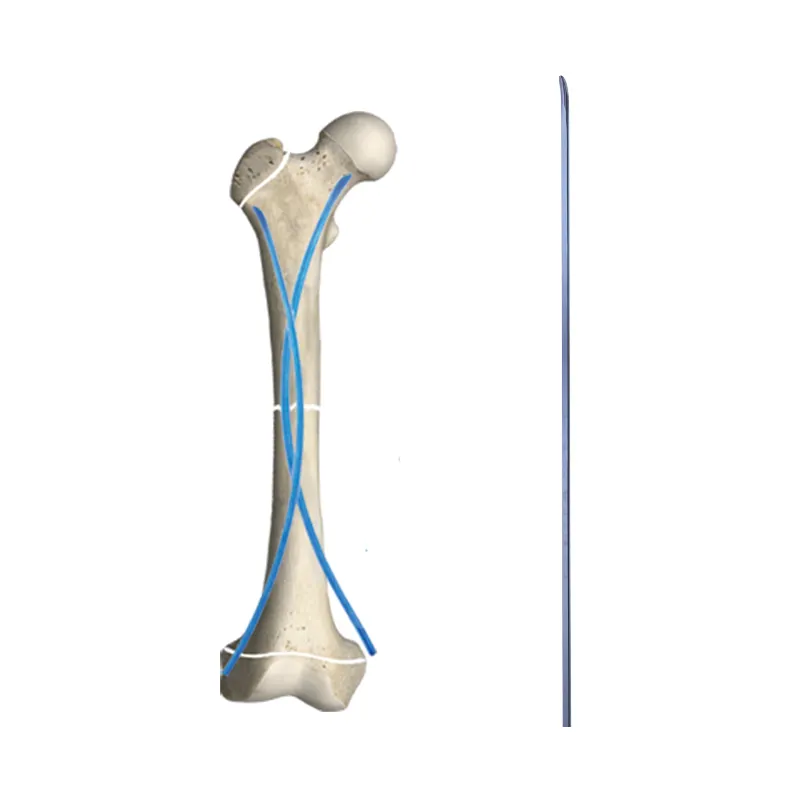
Intramedullary nails are a revolutionary technology in the field of orthopaedic surgery, which is useful for the treatment for bone stabilization. They can be placed in the medullary canal of long bones acting as endosteal support out of the bone. As a result of its intramedullary nail technology, soft tissues and vascular structures are less disrupted during surgery which results in less pain and quicker recovery.
Intramedullary Nails Intramedullary nailing has been shown to shorten recovery time and improve function in fracture patients. These nails are reported to offer good, stable internal fixation, thus minimising the risk of mal-alignment and non-union, common complications in other forms of fixation. Patients' rehabilitation is faster and they return to their daily routine knowing how to avoid a second injury when recovering from fractures.
Due to they are versatile the implants can be used in more complex fractures through a wide range of type of bone, increasing the surgical possibilities. Additionally, internal fixation using an intramedullary nail can be utilized for the femur, tibia, humerus, and even the clavicle, giving orthopedic surgeons multiple options geared to specific disease processes and individual patient characteristics. This adaptability is important when dealing with complex fractures that may be less responsive to standard techniques.
Early Applications: From Spinal Fractures to Long Bone Stabilization
Historical Development of Intramedullary Fixation
Screw fixation was first introducted in the 1940s and the role of orthopedic surgery has undergone a great transformation from the methods of treatment carried on the back. This new method was initiated by German surgeon Gerhard Küntscher demanding development of the oldest unreamed (first generation) non-locked nail. These stainless-steel implants achieved stable osteosynthesis with bone flexible impingement and no reliance on external fixation was necessary. This transition led to marked increase in union rates and fewer complications, a point confirmed by many historical series.
By the 1950s, additional developments such as intramedullary reaming pioneered by Albert Wilhelm Fischer, were developing. This led to bigger nails with more cortical contact and therefore better implant stability. These fundamental breakthroughs set the stage for orthopedic advancements, robust surgical procedures with higher success.
Pioneering Use in Vertebral and Femoral Fractures
The leading use of intramedullary nails in vertebral and femoral fractures proved their value in the treatment of challenging injury patterns. In the 1960s, Robert Zickel evolved this technique by designing the first cephalomedullary nail for proximal femur fractures. This would help in offering better treatment, leading to early recovery with least complications. This early success helped in generating helpful evidence that can drive current practice, including the development of closed nailing techniques due to advances in radiological imaging.
Notably, the outcomes from these cases highlighted several critical benefits; among them were reduced surgery duration and minimized postoperative complications. As technology evolved, intramedullary nails continued to shape orthopedic practices by expanding treatment possibilities for long bone fractures and influencing a paradigm shift towards internal stabilization over traditional methods.
Technological Evolution: Materials, Design, and Biomechanics
Advancements in Implant Materials: Titanium vs. Stainless Steel
Recent improvements of implant materials have put much focus on the application of titanium and stainless steel in orthopedics. There are a number of pros and cons to each material that can influence surgical results. Titanium is famous for its high biocompatibility and corrosion resistance and it is widely used by many surgeons. Stainless steel, on the other hand, is not for all applications, and is both cost-effective and provides relatively high strength, and is therefore the material of choice for some applications. Clinical researches have demonstrated the fact that the selection of materials plays a pivotal role on the longevity of the implant and patient outcome, suggesting that an appropriate selection of material is important for the cases.
Innovations in Nail Geometry and Locking Mechanisms
Advancements in nail geometry and interlocking technology have greatly increased the flexibility of the design and have rendered the nail more anatomically friendly, allowing for more specific patient-based needs to be addressed in orthopaedic surgery. Advancements now consist of nails in different sizes and lengths that enable the orthopedist to work with a variety of fractures. Advanced locking implants that enhance stability against motion are important for healing of fractures. These design aesthetics are substantiated with biomechanical analysis which show substantial improvement in load distribution. By addressing these factors, intramedullary nails achieve efficient fracture stablization and maximal fracture healing.
Biomechanical Optimization for Load Distribution
Biomechanical optimization is about optimal distribution of mechanical loads-important for stimulating bone-formation by callus. Studies show that proper distribution of load greatly reduces regions of stress concentration on the bone and improves healing time. The biomechanics-based designs have been reported to improve clinical performance and decrease failure rate of implants. These improvements help spread the mechanical stresses of healing over a greater area, promoting healing and reducing the likelihood of complications. The development of biologically-friendly implant profile such as these with biomechanically optimized design highlights the progressive nature of intramedullary nail technology.
Expansion to Joint End Fixation: Redefining Surgical Boundaries
Adaptation for Periarticular Fractures: Hip and Ankle Innovations
There has been a relatively high degree of conversion of intramedullary nails to treat periarticular fractures, particularly those around high load joint regions like the hip and ankle. This development process is necessary, as periarticular fractures demand specific management based on their proximity to joint surfaces. Advancements have resulted in special nails being created to optimize stability and adaptation in these regions. For example, the newer implant designs incorporate special geometries and locks that take into account the biomechanical environment in joint areas. Clinically, these advancements have been supported in that they have led to better results in fracture care and faster postoperative recovery. Such a turn is of further significance to patients who suffer from complicated fractures due to the localising and structural aspects, highlighting the importance of focused and efficient answers.
Dynamization Techniques in Metaphyseal Regions
Dynamization methods are used in the management of metaphyseal fractures, resulting in increased stability and the ability to adjust the healing process. These methods apply tension changes and encourage physiological loading that replicates normal healing mechanisms of bone and thus accelerates healing. These interventions are particularly attractive especially in places where traditional stabilization techniques may be inadequate, on account of the diverse and irregular structures of bones. Clinical research suggests that dynamization can increase healing rates in patients, as it permits controlled mobility and stress at the fracture, which is essential for bone healing. Through enabling for efficient load sharing with less rigidity dynamization methods promote the biological healing response and enhance surgical results.
Clinical Advantages of Modern Intramedullary Systems
Enhanced Stability Through Controlled Fracture Compression
The latest intramedullary systems add an important tool to the fracture treatment options with controlled, compressive fracture management to provide increased stability and promote healing. This would be a technique where the ideal amount of pressure is applied to the fracture site to encourage better alignment and stability. These compressive techniques have been shown to reduce healing time dramatically while also reducing the risk of poor patient outcomes by stabilizing the fracture environment. This progress epitomizes the importance of new technologies and associated new techniques in the overall treatment of fractures.
Minimally Invasive Approaches and Reduced Soft Tissue Damage
Reducing of soft tissue injury is a major advantage of the minimally invasive technology used in most of the intramedullary systems. Exactly these concepts create a refinement of surgical preparation that minimizes scarification and postoperative recovery times. Patients enjoy less postoperative pain and shorter hospital stays based on clinical data. These methods change the recovery experience for patients, while they are designed to preserve soft tissue and promote better long-term results.
Accelerated Healing and Functional Recovery Outcomes
The new intramedullary systems support rapid healing times, so patients recover faster and get back to their activities. This technique not only accelerates the osteosynthesis but also provides better functional results because the nails form a stable bed. A relatively large body of clinical evidence supports the efficacy of such systems, providing optimized patient survival and quality of life. These innovations underscore the potential of intramedullary nails to have great influence on the rehabilitation of the patient as a whole.
FAQ
What are intramedullary nails?
Intramedullary nails are surgical implants used in orthopedic surgery to stabilize fractures by inserting them into the medullary canal of long bones.
How do intramedullary nails promote quicker recovery?
Intramedullary nails offer internal fixation, which enhances fracture alignment, reduces non-union risks, and allows for faster rehabilitation and return to normal activities.
What types of fractures can be treated with intramedullary nails?
Intramedullary nails can treat complex fractures of the femur, tibia, humerus, and clavicle, providing surgeons with flexible options.
What advancements have been made in intramedullary nail technology?
Recent innovations include improved materials like titanium, advanced nail geometry, and locking mechanisms to enhance surgical adaptability and optimize load distribution.
How do minimally invasive techniques benefit surgical procedures?
Minimally invasive techniques reduce soft tissue damage, improve recovery times, and result in less postoperative pain and scarring.
Table of Contents
- The Role of Intramedullary Nails in Modern Orthopedic Surgery
- Early Applications: From Spinal Fractures to Long Bone Stabilization
- Technological Evolution: Materials, Design, and Biomechanics
- Expansion to Joint End Fixation: Redefining Surgical Boundaries
- Clinical Advantages of Modern Intramedullary Systems
- FAQ